For some time, reproductive biologists have been investigating whether mammals require gender differentiation for reproduction or if it is theoretically possible for mammals to arise from a single cell, similar to the origins of early life forms. In simple terms, exploring the possibility of creating mammals, including humans, using only male cells without the need for female counterparts in the reproductive process. This inquiry delves into the complexities of sexual reproduction, genetic diversity, and the evolutionary implications of asexual processes. While initially appearing paradoxical for some, this inquiry resides firmly within the realm of biological sciences.
And that is precisely what researchers of Kyoto University, Mitinori Saitou’s and his team were trying to achieve. The team has been researching the possibilities of the generation of human oogonia (precursor cells that produce “eggs” in the fetus) from induced pluripotent stem cells (iPSCs) using purely a so called “in vitro gametogenesis“(IVG) approach . iPSCs are a specific type of stem cells that have the potential to develop into almost any cell type within the human body. The IVG method allows scientists to artificially nurture ordinary cells, such as skin cells—or in this case, iPSCs—to develop into eggs or sperm by reprogramming them and guiding them through the steps of germ cell development, and in 2018 the team of researchers achieved a groundbreaking milestone by successfully creating cells that mimicked human fetal oogonia, indicating potential for creating human germ cells beyond early stages. Mitinori’s team achieved this breakthrough and published their research; “Generation of human oogonia from induced pluripotent stem cells in vitro” in Science on October 19, 2018, however, due to the technological limitations at the time, the reliance on xenogeneic(mouse-derived) support for further development, and ethical considerations, the experiment demonstrated an important proof-of-concept but did not yet enable complete in vitro maturation of functional human eggs.
Generation of human oogonia from induced pluripotent stem cells in vitro by Chika Yamashiro and Mitinori Saitou
The study involved differentiating iPSCs into primordial germ cell-like cells (hPGCLCs) using growth factors, which were then cultured with mouse ovarian cells to form xenogeneic reconstituted ovaries for up to 120 days. The resulting cells mimicked human fetal oogonia, achieving crucial epigenetic changes and proliferation but not full meiosis. The team used both male (XY) and female (XX) donor iPSCs, showing potential for creating eggs from male cells. This significant milestone indicated the potential for creating human germ cells beyond early stages, although limitations exist due to reliance on mouse cells and low efficiency.
While Saitou’s lab has achieved a partial of success, the research has been subject to moral and ethical limitations, when it comes to executing the study on humans or similar mammals, they were unable to progress to full meiosis or mature oocytes in this setup, and the researchers stopped at the pre-meiotic oogonia stage. Yet This 2018 work has become a foundation for further research, and the team is still actively attempting to build upon it in the very same institution, focusing on completing meiosis and achieving mature human gametes. Nevertheless, due to Japan’s advancing regulatory framework, changes introduced in 2023 enabled further progression toward embryo creation from these lab-grown cells, allowing researchers to extend similar methods to cynomolgus monkeys, inducing fetal-like meiotic oocytes from embryonic stem cells.
Building upon this foundation scientists at Oregon Health & Science University (OHSU) published a study titled Induction of experimental cell division to generate cells with reduced chromosome policy in September 2025 in Nature Communications demonstrating a technique to further elevate the IVG method generating functional human egg cells (oocytes) from skin cells. Their approach involves somatic cell nuclear transfer (SCNT) process, similar to that used in 1997 to clone Dolly the sheep. The researchers used a nucleus from a donor skin cell, and inserted it into a human egg cell that has had its own nucleus removed. This creates a hybrid cell with the donor’s DNA in an egg-like environment and can be triggered to mimic meiosis, halving the chromosome count to produce an immature egg with 23 chromosomes by a chemical process called “mitomeiosis“. The egg then fertilized with sperm via intracytoplasmic sperm injection (ICSI). The research has successfully produced 82 eggs and fertilized some to develop them into early embryos up to the blastocyst stage. Although developmental success was achieved, all the embryos had chromosomal abnormalities such as incorrect numbers or unpaired chromosomes , so they were unable to prove the concept viable for implantation or further development.
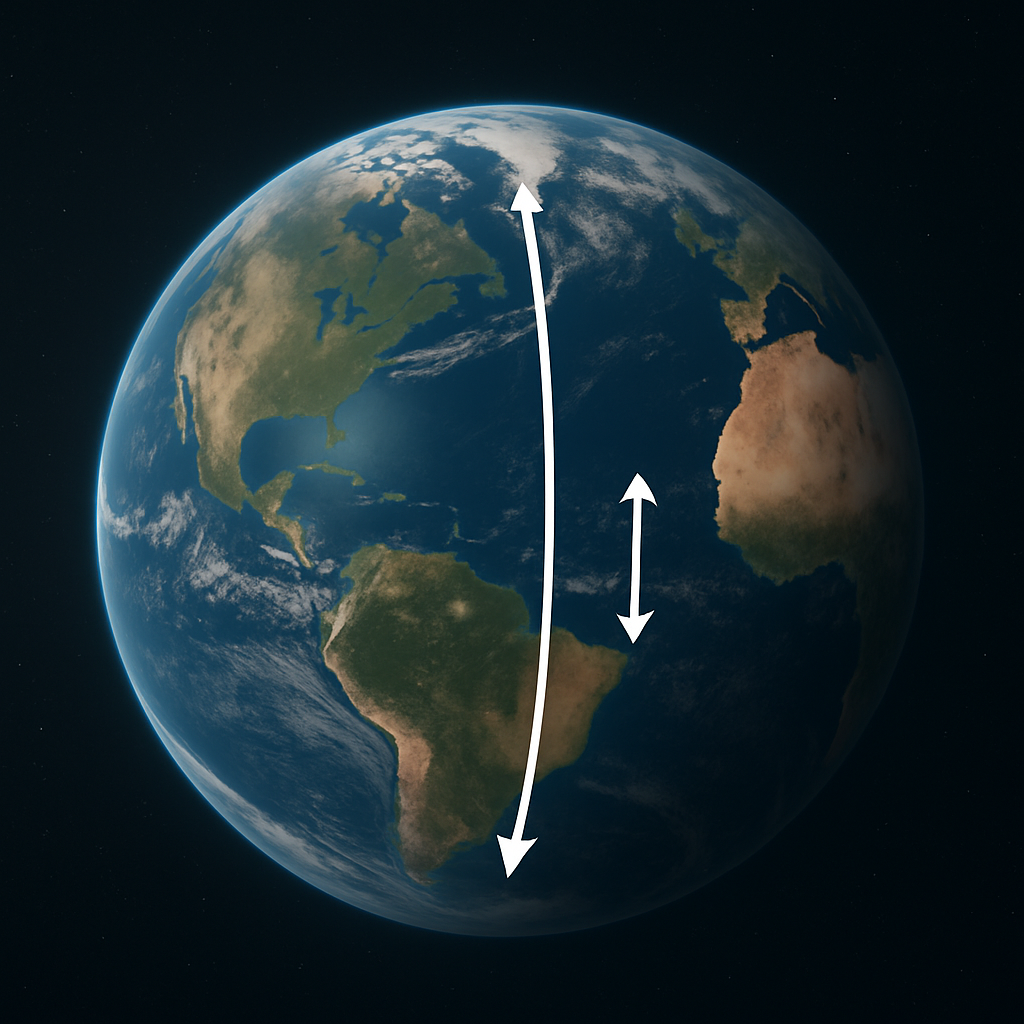
In the case of the Oregon study, scientists used skin cells from female donors, however, the method is designed to work with male cells too, based on successful animal models, opening the door for applications such as developing a child from two genetically unrelated males: one man’s skin cell for the generation of the egg and one for the fertilization. While each of these experimental research studies differs to an extent, and the OHSU model required an official donor egg which was later modified, the collaboration of these foundational models could potentially create possibilities for cultivating mature human gametes and developing them into a healthy fetus without the need for female DNA or reproductive organs.
To stay informed about the ethical and legal hurdles concerning IVG and to follow the active research in in vitro gametogenesis and stem cell biotechnology, subscribe to our newsletter or explore the latest studies published in the leading journals Nature Communications and Science.

Subscribe to continue reading
Subscribe to get access to the rest of this post and other subscriber-only content.